This article may contain affiliate / compensated links. For full information, please see our disclaimer here.
Living with an autoimmune disease is a complex journey that affects not only physical health but also mental and emotional well-being. Autoimmune diseases, such as rheumatoid arthritis (RA), lupus, multiple sclerosis (MS), and inflammatory bowel disease (IBD), are characterized by chronic inflammation and immune system dysregulation. These conditions often come with significant psychological challenges, including depression, anxiety, cognitive dysfunction, and social isolation. Despite the growing recognition of the connection between autoimmune diseases and mental health, this aspect of care remains underexplored in many clinical settings. This article delves into the mental health impact of autoimmune diseases, the biological and social mechanisms involved, and actionable strategies to improve emotional well-being.
Autoimmune diseases are physically debilitating, but their mental health impact can be equally profound. Patients often face a dual burden: managing the physical symptoms of their condition while navigating the emotional challenges that accompany chronic illness.
Pain and fatigue are among the most reported symptoms in autoimmune diseases. Chronic pain not only disrupts daily life but also has a direct link to mood disorders:
Autoimmune diseases are unpredictable. Flare-ups can occur without warning, making patients feel like they have little control over their health. This uncertainty often leads to:
Cognitive dysfunction, or “brain fog,” is a common symptom in many autoimmune diseases. It includes:
Many patients report feeling isolated due to their condition:
The connection between autoimmune diseases and mental health disorders is not solely psychological; it is deeply rooted in biology. Shared mechanisms between these conditions provide valuable insights into why they often co-occur.
Inflammation is central to autoimmune diseases and plays a significant role in mental health disorders:
In some cases, inflammation directly affects the brain:
Autoimmune diseases can disrupt hormonal pathways:
The gut microbiome plays a crucial role in regulating inflammation:
The prevalence of mental health issues among individuals with autoimmune diseases is alarmingly high. Below is a table summarizing key statistics:
| Autoimmune Disease | Depression (%) | Anxiety (%) | Cognitive Dysfunction (%) |
|---|---|---|---|
| Rheumatoid Arthritis | 74% | 50% | 30% |
| Lupus | 64% | 60% | 40% |
| Multiple Sclerosis | 50% | 45% | 70% |
| Inflammatory Bowel Disease | 40% | 35% | 25% |
These figures highlight the urgent need for integrated care models that address both physical symptoms and mental health challenges.
The social dimension of living with an autoimmune disease adds another layer of complexity to mental health outcomes.
Autoimmune diseases are often invisible illnesses. Symptoms like pain or fatigue may not be outwardly apparent, leading others to dismiss or underestimate their severity:
Chronic illnesses come with significant financial burdens due to medical bills, lost income from missed workdays, or disability-related expenses. Financial stress compounds feelings of anxiety and depression.
Living with an autoimmune disease can strain personal relationships:
While living with an autoimmune disease presents undeniable challenges, there are actionable strategies that can help improve mental well-being:
Engaging with healthcare professionals who understand both physical and psychological aspects of chronic illness is crucial:
A strong support system is invaluable for emotional resilience:
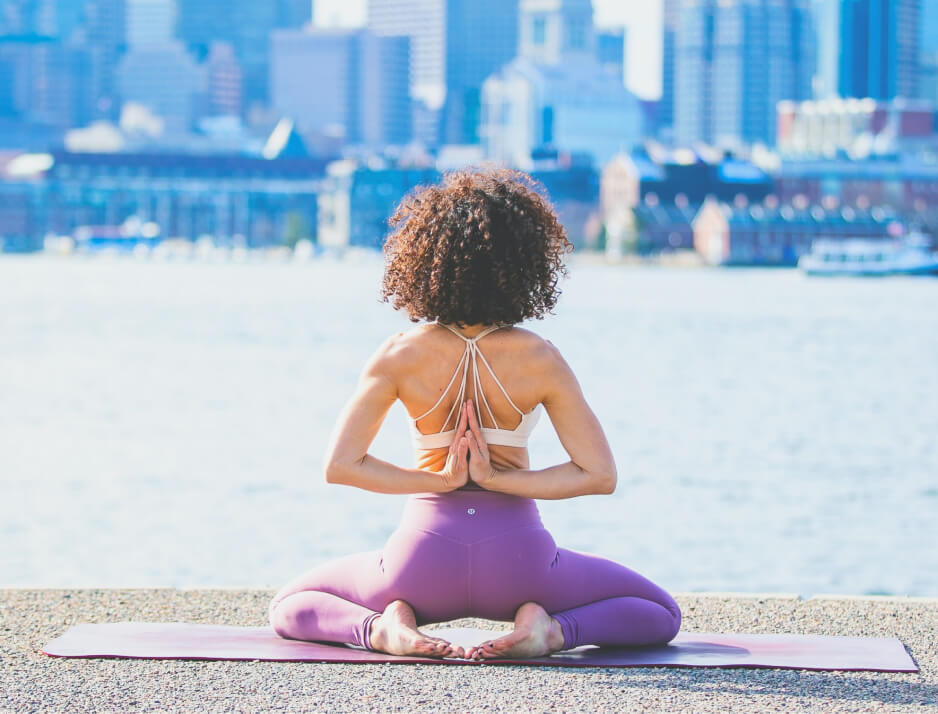
Mindfulness-based interventions like meditation or yoga have been shown to reduce stress and improve mood:
Adopting an anti-inflammatory lifestyle can reduce both physical symptoms and mood disturbances:
CBT helps reframe negative thought patterns associated with chronic illness:
Despite clear evidence linking autoimmune diseases with mental health disorders, care remains fragmented:
To address these gaps:
Living with an autoimmune disease is not just a physical challenge—it profoundly impacts mental health as well. From chronic pain and fatigue to social isolation and stigma, these conditions affect every aspect of life for those who live with them. By understanding the biological underpinnings of this connection and addressing social factors through holistic care models, healthcare providers can better support patients’ emotional well-being alongside their physical health needs. Patients themselves can take proactive steps by seeking professional help, building support networks, adopting mindfulness practices, and making anti-inflammatory lifestyle changes. Ultimately, recognizing the interplay between autoimmune diseases and mental health is essential for improving quality of life—and ensuring that no one faces these challenges alone.

Gemma is a dedicated clinician who manages her own multiple sclerosis (MS) with resilience and expertise. In addition to her medical practice, she holds a degree in philosophy, providing her with unique insights to navigate complex and challenging situations.